- Visibility 19 Views
- Downloads 0 Downloads
- DOI 10.18231/j.ijcaap.2024.034
-
CrossMark
- Citation
Urolithiasis: Mechanism of stone formation, diagnostic modalities and treatment protocols
Introduction
Nephrolithiasis or urolithiasis, commonly referred as kidney stones or renal calculi, are solid concretions or crystalline aggregations that form within the kidneys due to mineral deposition from urine. Kidney stones are typically expelled from the body through the urinary tract without symptoms in many cases. However, if stones grow to a size of at least 3 millimetres, they can obstruct the ureter. Ureteral obstruction leads to post-renal azotaemia, hydronephrosis (distension and dilation of the renal pelvis and calyces), and ureteral spasm, causing intense pain known as renal colic. Renal colic is typically felt in the flank (the area between the ribs and hip), lower abdomen, and groin, and may be associated with symptoms such as nausea, vomiting, fever, haematuria (blood in the urine), pyuria (pus in the urine), and dysuria (painful urination). The pain of renal colic often comes in waves lasting 20 to 60 minutes, starting in the flank or lower back and radiating towards the groin or genital area.[1]
The incidence and recurrence of kidney stone disease are rising globally, and there are few effective treatment options. Approximately 12% of people worldwide will experience urolithiasis at some point in their lives. It affects people of all ages, genders, and races; however, in the 20–49 age range, men are more likely than women to experience it. Though the incidence of nephrolithiasis is rising in girls, the lifetime recurrence rate is higher in males.
According to recent studies, urolithiasis has become more common in both industrialized and developing nations over the past few decades. It is thought that changes in food and lifestyle choices, such as less physical activity, are linked to this expanding tendency. Kidney stones afflict 1 in 11 persons in the US. About 12% of Indians are predicted to develop urinary stones, and of those, 50% may lose their ability to function as kidneys.[2]
Epidemiology of Kidney Stones
Urolithiasis affects approximately 12% of the global population at some point in their lives, affecting individuals across diverse demographics including age, sex, and ethnicity, with a higher prevalence noted among men aged 20-49 years. Despite this, males exhibit a greater lifetime recurrence rate, even as nephrolithiasis incidence rises among females. Therefore, proactive management strategies are imperative for effective urolithiasis control. Recent studies indicate a consistent rise in urolithiasis prevalence globally, spanning developed and developing nations alike. This trend is associated with lifestyle modifications such as decreased physical activity, dietary changes, and broader environmental factors like climate change. Within the Indian population, around 12% are projected to develop urinary stones, with half of these cases potentially leading to impaired kidney function.[3]
The aetiology of kidney stone
Metabolic Factors: Imbalances in urine composition can lead to the formation of crystals that aggregate into stones. Factors such as hypercalciuria (high calcium levels in urine), hyperoxaluria (high oxalate levels), hyperuricosuria (high uric acid levels), and hypocitraturia (low citrate levels) contribute significantly.
Genetic Predisposition: Certain genetic disorders, such as cystinuria and hyperoxaluria, increase the risk of kidney stone formation. These conditions affect the metabolism of substances like cystine and oxalate, making their excretion more likely to form stones.
Environmental Factors: Environmental factors, such as climate (hot and dry climates can lead to dehydration and concentrated urine), occupation (involving exposure to certain chemicals), and geographical location (areas with high incidence rates due to water composition), play a role in stone formation.
Dietary Factors: High intake of oxalate-rich foods (like spinach and nuts), purine-rich foods (increasing uric acid production), and sodium can contribute to stone formation. Inadequate fluid intake reduces urine volume, increasing the concentration of stone-forming substances.
Anatomical Factors: Structural abnormalities in the urinary tract, such as narrow ureters or kidney malformations, can obstruct urine flow and promote stone formation.
Medical Conditions: Certain medical conditions, such as recurrent urinary tract infections, inflammatory bowel disease, and metabolic disorders like hyperparathyroidism, increase the risk of kidney stone development.[4]
Causes of Urinary Tract Stone Formation
Urinary tract infections, inadequate excretion of urine, and nutritional imbalances resulting from excessive calcium and oxalates consumption are some of the factors that can cause stones to form. Vitamin abnormalities, such as deficiencies in vitamin A or excess vitamin D, and metabolic diseases such as hyperthyroidism, cystinuria, gout, and intestinal dysfunction, can also lead to kidney stones and urolithiasis. This intricate mechanism arises from an imbalance between the kidneys' promoters and inhibitors.
The pathogenesis of illnesses, including urolithiasis and kidney stone formation, is caused by two basic factors:
Higher excretion of components that contribute to the formation of stones in the urine, including calcium, phosphorus, uric acid, oxalate, and cysteine.
Physicochemical changes that affect the formation of stones, such as the pH of the urine, the properties of the stone matrix, and the presence of protective compounds in the urine.
For a stone to form, urine must meet the requirements for precipitating crystalline structures. Along with other variables that can alter nucleation, crystallization, and aggregation, urine pH is a significant factor that influences the formation of stones.[5]
Symptoms and indicators of urolithiasis illnesses
Kidney stone symptoms differ depending on whether the stone is located inside the kidney, ureter, or bladder. Stone growth does not initially result in any symptoms. Subsequently, haematuria (bloody urine), renal colic (severe cramping pain), flank pain (pain in the back), urinary tract infections, obstruction of urine flow, and hydronephrosis (dilation of the kidney) are signs and symptoms of stone illness. These ailments may cause nausea, vomiting, and the stone event that goes along with it.[6]
Kidney stone symptoms include
Colicky pain
Nausea/vomiting
Haematuria
Pyuria
Dysuria
Oliguria etc
Conventional treatment and prevention of urolithiasis diseases
For treatment of urolithiasis various types of procedure is carried out.
Surgical treatment likes
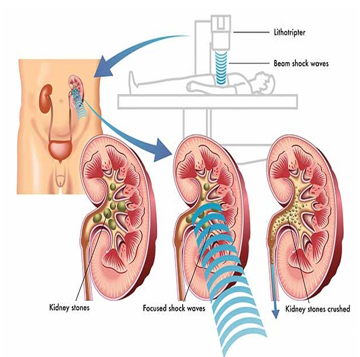
Shock wave treatment which is the only non-invasive treatment for stone disease,
Endoscopic process, ureteroscopy and percutaneous nephrolithotomy provides an efficient way to treat stones. The severe nature of renal colic has promoted a lower threshold at which narcotic analgesic, thiazide like diuretic and potassium citrate is prescribed.
Foods that enhance the risk of calculi formation
Organic acids rich foods (oxalates like spinach, rhubarb, nuts and wheat bran.
Alcohol, Beer and wine to a little extent as they contain purines High intake of salt.
Foods that inhibit calculi formation
Lemon and citrus fruit juice, coffee, tea and citrates rich soft drinks
Foods like as radish, beet root and horse gram
Low protein diet and rich fibre foods
Others like Vitamin E, B6, and magnesium
Low salt diets
Available treatments
Medicine therapy
Like as Thiazide diuretics (e.g. Hydrochlorothiazide), Alkali (e.g. Potassium citrate), Allopurinol, Sodium cellulose phosphate (SCP), Penicillamine (Cuprimine), Analgesic (Diclophenac sodium), Bisphosphonates, Potassium phosphate, Oxalobacter Formigenes and other probiotics etc.
Surgical therapy
Like as Extracorporeal Shock Wave Lithotripsy, Percutaneous Nephrolithotomy, Ureteroscopic stone removal etc.
Herbal therapy
Like as Cystone, Calcuri, Chandraprabha bati, Trinapanchamool, Rencare Capsule, Patherina tablet, Ber Patthar Bhasma, Chander Prabha vati etc.[7]
Herbal folk drugs produce following actions such as:
Diuretic activity (Beneficial in increasing the urinary volume that allows the easy passage of small calculi out of the body in urine)
Crystallization inhibition activity (Helps to inhibit the different stages of stone formation by maintaining the balance between inhibitors and promoters of stone formation)
Lithotriptic activity (Avoid binding mucin of calculi to prevent crystal aggregation to form a large stone), analgesic and anti-inflammatory activities (Helps to escape the symptoms of stone formation)
Anti-oxidant activity (Prevent renal tissue injury , Anti-microbial activity (Prevent the occurrence of infections [8]
Herbs also improve the renal function and regulate oxalate metabolism which help in reducing the re occurrence of renal calculi.[9]
Pathogenesis of renal stone formation
The physical process of kidney stone formation involves a complex cascade of events initiated by crystal growth leading to stone development. The formation process is influenced by factors such as urine volume and the concentrations of calcium, phosphate, oxalate, and sodium ions. Conditions favoring high ionic concentrations, low urinary volume, acidic pH, and low citrate levels promote the formation of urinary calculi. The pathogenesis of kidney stone formation results from multifaceted physicochemical processes. Genetic, metabolic, environmental, and dietary factors play roles in urolithiasis pathogenesis, all predisposing to salt crystallization within renal tubules. Crystalluria is commonly observed in normal individuals, where crystals remain dispersed and are flushed out by urine flow. However, under certain chemical and electrical conditions, crystals can aggregate. Once aggregated, crystals adhere to epithelial surfaces, facilitating their growth and eventual formation into kidney stones.[10]
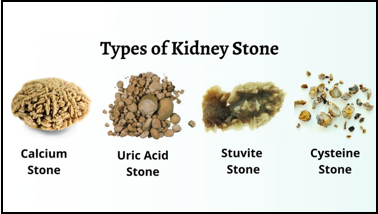
Types of kidney stones
Urinary stones are typically classified based on their chemical composition (calcium-containing, struvite, uric acid or other compounds).
Calcium stones
Calcium stone can exist as calcium oxalate or calcium phosphate or calcium carbonate. Among all the types these are the prominent ones constituting around 70–80% of the total stone forms. Calcium oxalate can exist as calcium oxalate monohydrate (COM) or dihydrate (COD). COM is the more stable form and common compared to the COD. Various factors may contribute to calcium stone such as hypercalciuria, hyperoxaluria, hyperuricosuria etc.
Uric acid or urate stones
Uric acid stone accounts approximately for 5–10% of all the types of stones. High purine content of diet such as animal protein is main risk factor for the formation of uric acid stone. Other risk factors are low urine volume, hyperuricosuria, and low urinary PH.
Magnesium ammonium phosphate stones or struvite stone
Also called as infection stones or triple phosphate stones. These stone occur at the extent of 12–15%. The main cause for the struvite stone is urinary tract infections where urease produced by microbes split urea into ammonia and carbon dioxide. This makes the urine alkaline and makes phosphate insoluble at its high pH. Thus, phosphate gets precipitated on the ammonia leading to the stone formation. Its more common in female compared to male.
Cystine stones: The occurrence of cysteine stone is less than 3% among all the types of the stones. It occurs as a genetic disorder with defect in cystine amino acid transportation, which results in excess excretion of cystine in urine referred as cystinuria. It is an autosomal recessive disorder resulting in impaired renal tubular absorption of cystine and excretion of cystine in urine. As cystine is insoluble in urine results in the formation of stones in kidney.
Drug-induced stones: These stone accounts for only 1% of total stones. Drugs such as triamterene, atazanavir, and sulfa drugs induce stone formation. Lithogenic drugs and their metabolites may get deposited to form nidus or on already existing stone. Some drugs may also interfere in purine and calcium oxalate metabolism and may lead to the stone formation.[11], [12]
Mechanisms of Renal Stone Formation
Kidney stone pathogenesis, also known as biomineralization, is a complicated biochemical process that is still poorly understood. The biological process of renal stone development includes urine supersaturation and physicochemical alterations. A solution is said to as supersaturated if it has more dissolved material in it than the solvent could normally dissolve. Supersaturation causes solutes to precipitate in urine, which triggers nucleation and the formation of crystal concretions. In other words, crystallization happens when two ions' concentration in a solution is higher than their saturation point. The pH and particular quantities of excess chemicals have an impact on the transition from a liquid to a solid phase. Risk factors for crystallization include low urine volume and the amount of urinary saturation with regard to the components that form stones, such as calcium, phosphorus, uric acid, oxalate, and cystine. Thus, the kinetics of a supersaturated solution which includes the rates of nucleation or crystal growth and thermodynamics, which causes nucleation, are what drive the crystallization process. Therefore, avoiding supersaturation can help prevent lithiasis.
It should be highlighted, nonetheless, that the degree of imbalance between urinary inhibitors and crystallization promoters usually determines the formation of stones The process by which stones form in the kidneys involves crystal nucleation, growth, aggregation, and retention.[13], [14]
Promoters of stone formation
Several receptors play crucial roles in kidney crystal retention. In a CaOx monohydrate (COM) model, 1,141 differentially expressed proteins (DEPs) were identified in COM-treated HK 2 cells. Proteins like CD44, nucleolin, hyaluronan (HA), heat shock protein 90 (HSP90), Annexin II, and osteopontin (OPN) modulate stone formation. Receptors include phosphatidylserine and acidic side chains of proteins, promoting crystal attachment. Calcium, oxalate, urate, and phosphate ions promote crystallization and aggregation. First-time nephrolithiasis patients show elevated serum calcium and 1,25(OH)2D levels, implicating altered calcium and vitamin D regulation in stone formation. Higher serum calcium, regulated by calcium sensing receptor (CaSR), promotes lithogenesis. Urate and phosphate ions enhance crystal attachment. Urine pH affects CaOx crystallization, with low pH promoting precipitation and high alkaline pH promoting nucleation. Lysozyme and lactoferrin accelerate COM crystal growth by increasing surface layer advancement rate. [15]
Inhibitors of stone formation
Normal urine contains inhibitors that reduce crystallization and inhibit crystal aggregation/adhesion to tubular epithelial cells. These inhibitors include anions (e.g., citrate), metallic cations (e.g., magnesium), and macromolecules (e.g., OPN, THP, UPTF 1, NC, serum IαI subunits). Citrate, at concentrations above 0.1 mM, efficiently inhibits crystal growth, yet many nephrolithiasis patients exhibit decreased citrate excretion. Alkali supplements are used to treat hypocitraturia by restoring citrate excretion. Metallic cations like magnesium synergistically inhibit crystal growth in acidic environments. Despite these inhibitors, competition with crystallization promoters ultimately determines crystalluria patterns in nephrolithiasis and healthy individuals. Increased promoters and reduced inhibitors contribute to crystal formation and kidney stone occurrence. [15]
Nucleation
Nucleation initiates solid crystal formation in a solution, marking the onset of stone formation in the kidney. Supersaturation describes a solution with more dissolved material than typical solvency allows. Crystal nucleation, crucial in renal stone genesis, can occur homogeneously within unstable supersaturation zones or heterogeneously induced by promoters on pre-existing surfaces, lowering the energy needed for crystallization. As crystals grow, the solution's free energy diminishes as more components integrate into the crystal structure. Crystalline particles can bind in oriented or random patterns, expanding into larger structures.
Crystal growth
Following nucleation, microcrystals undergo epitaxial crystal growth, where one crystalline material aligns and grows on another substrate's lattice. This process includes monoepitaxial growth, where molecules or ions adsorb sequentially onto a crystal surface from supersaturated urine, and heteroepitaxial growth, where crystals develop directly on surfaces with different compositions. In a supersaturated liquid, atoms or molecules begin clustering, with surface energy increasing the total free energy, especially in smaller clusters. Crystal growth depends on molecular size, shape, material properties, pH, and structural defects, all crucial factors in particle formation.
Aggregation
Aggregation involves crystal nuclei binding to form larger particles, aided by further salt addition. Close inter-particle distances increase attractive forces, favouring particle aggregation. This process is pivotal in stone formation, where aggregation often outweighs nucleation and growth stages. Aggregation dynamics in solution are influenced by forces balancing aggregation and disaggregation effects, alongside inter-particle distances promoting aggregation.
Retention
Crystal retention can be caused by the association of crystals with the epithelial cells lining. Urolithiasis requires formation of crystals followed by their retention and accumulation in the kidney. Another process that may lead to stone formation is crystal retention. i.e., crystal precipitation, growth, and aggregation, which results in urinary stone formation, if the nucleated crystals were flushed out by urinary flow. Retention might also depend on the composition of the renal tubular epithelial cell surface. [15]
Pharmacological agents used for the treatment of urolithiasis
Once the presence of urinary stones is confirmed and their location, size and types are established, medical intervention comes into play that includes treatment by drug therapy or surgical removal of the stones depending upon their size, shape, location, type and other pathological conditions.
Thiazide and related diuretics are indicated in renal stone disease associated with hypercalciuria. They are known to produce hypocalciuric action by enhancing reabsorption of calcium at proximal and distal convoluted tubule. Problem with the use of thiazide diuretics is their universally known potassium depletion causing hypokalaemia, which can ultimately lead to hypocitraturia, a factor responsible for augmenting urolithiasis, which could be corrected by potassium citrate or amiloride supplementation. Potassium-sparing diuretic, triamterene can also be used to correct hypokalaemia but it possesses the risk of producing triamterene stone, a type of drug stone owing to its low solubility.
Allopurinol is prescribed for the treatment of calcium oxalate and uric acid stones. Being a xanthine oxidase inhibitor, it inhibits uric acid production from hypoxanthine and xanthine thus reducing urate levels in urine, which again turns out to be inhibitory for nucleation of calcium oxalate. Febuxostat is also a xanthine oxidase inhibitor like allopurinol but has been found to be more efficacious in reducing urinary urate levels as compared to allopurinol.
Potassium citrate basically raises urinary citrate levels. Citrate complexes urinary calcium to a soluble form, thus inhibiting calcium phosphate and calcium oxalate crystal aggregation. Potassium citrate also tends to inhibit uric acid stone formation owing to its alkalinizing effect on urine. Unlike sodium citrate and sodium bicarbonate, it does not tend to raise sodium load, which is known to increase calcium excretion and produce citrate reduction in urine and is therefore preferred over them. But it does possess tendency for producing gastrointestinal upset. Potassium citrate, allopurinol and thiazide diuretics are known to reduce stone recurrence rates as well.
Sodium cellulose phosphate is known to bind to intestinal calcium and thus inhibit absorption of calcium leading to reduction in the elevated calcium excretion thus reducing calcium stone formation. It has been found to be efficacious but has potential to cause hyperoxaluria and hypomagnesaemia, which again are vital for exacerbating renal stone disease. Sodium cellulose phosphate can also cause parathyroid stimulation.
D-penicillamine is used in case of cystine stones for treating cystinuria. By forming penicillamine-cysteine heterodimers that are comparatively more soluble than cysteine-cysteine homodimers, it promotes dissolution of cystine stones and lowers cystine levels in urine. However, it is of limited use owing to its potent adverse effects which include, nephrotic syndrome, leukopenia, thrombocytopenia, neuropathy, dermatitis and pancytopenia.
Acetohydroxamic acid is prescribed in case of struvite stones that are usually formed due to or are associated with the UTI caused by urease producing organisms. Acetohydroxamic acid being a urease inhibitor seems to be beneficial in these types of infection stones but its efficacy is challenged by its potential adverse effects that include deep vein thrombosis, haemolytic anaemia, gastrointestinal distress, tremors.[16]
|
Stone composition |
Common pathophysiological factor |
Drug |
|
Calcium containing stones |
Hypercalciuria |
Chlorthalidone |
|
Indapamide |
||
|
Hydrochlorothiazide |
||
|
Calcium oxalate or calcium phosphate stones |
Hypocitraturia |
Potassium citrate |
|
Primary hyperoxaluria |
Pyridoxine |
|
|
Hyperuricosuria |
Allopurinol |
|
|
Uric acid stones |
Low urinary pH |
Potassium citrate |
|
Hyperuricosuria or hyperuricemia |
Allopurinol |
|
|
Cystine stones |
Low urinary pH |
Potassium citrate. |
|
Cystinuria |
D-penicillamine, Tiopronin. |
Diagnostic Techniques
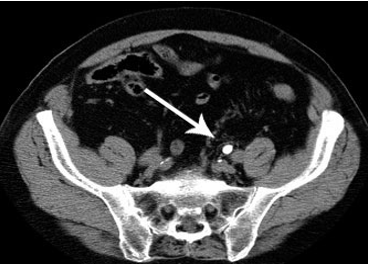
Computed tomography
CT can help locate stones of any type, size, or location. Patients on HIV therapy typically observe indinavir stones and pure matrix protein stones as the main exceptions. Moreover, CT can assess congenital urinary tract diseases, renal or urothelial neoplasms, and aid in identifying secondary obstruction indications like hydroureteronephrosis or perinephric edema. With its special capacity to differentiate between different types of stones, dual-energy computed tomography (DECT) can help predict how well extracorporeal shock wave lithotripsy (ESWL) will work for a certain stone type. CT scans remain the gold standard for identifying any remaining stone particles and monitoring post-treatment issues. Contrast-enhanced computed tomography can distinguish between phlebolith and distal ureteral calculus, as well as identify additional disorders that stone procedure CT may miss or only partially define. Furthermore, contrast-enhanced CT detected renal calculi of less than 3 mm with high sensitivity.[17], [18]
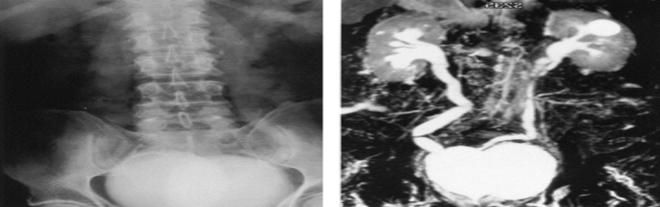
Ultrasonography
Ultrasonography (US) provides an accurate examination of the renal collecting systems, renal parenchyma, and bladder; however, imaging the ureters can be challenging, especially in patients with large intestinal gas or subcutaneous fat. Despite these limitations, US is a helpful initial imaging method, especially for people who are more vulnerable to radiation exposure, like children and expecting mothers, who frequently get urolithiasis. Even though they are not as accurate as CT scans, US and plain radiography can both rule out conditions like obstructive hydronephrosis and major recurring radiopaque urinary tract calculi.[19]

Magnetic Resonance Urography
Magnetic Resonance Urography (MRU) is a useful substitute for CT in the diagnosis and treatment of urolithiasis, despite its less common use. This is particularly true for patients who must minimize radiation exposure, such as children, pregnant women, or those with renal impairment who are intolerant of contrast agents. MRU aids in the identification and treatment of stones by providing a thorough evaluation of the urinary system's anatomy and the soft tissues that surround it. MRU can help distinguish between pathological and healthy ureteral obstruction, especially in pregnant women.[20]
Management
The stones' positioning and dimensions act as cues to initiate the management procedure. Asymptomatic persons with small stones (8 mm) may initiate conservative medical expulsive therapy (MET) management, including alpha-blockers and calcium channel blockers; these medications facilitate the passage of ureteral stones through the body and alleviate ureteral muscular spasms. However, open surgeries are being used less and less to treat ureteric stones, renal stones (20 mm), and lower renal pole stones (10 mm) because minimally invasive procedures like ureteroscopy (URS) and ESWL are becoming more and more successful. Furthermore, percutaneous nephrolithotomy (PCNL) can treat renal stones larger than 2 mm or lower renal pole stones less than 1 mm.[21]
Extracorporeal Shock Wave Lithotripsy (ESWL)
Introduced into clinical practice in 1980, ESWL is a minimally invasive technique for treating urinary stones with a success rate of 70–80% post-treatment. It is generally acknowledged as the favored course of therapy for small- to medium-sized stones (renal stones <20 mm or lower renal pole stones <10 mm), in accordance with worldwide norms. Many studies, including meta-analyses and randomized control trials, have shown that medical expulsive therapy can help ureteral stones pass during ESWL. This is especially true when used with alpha-blockers like tamsulosin. ESWL uses no aesthesia, takes less downtime than other modalities, and requires a shorter hospital stay. Although ureterorenoscopy has a higher recurrence rate than ureteroscopy, it is nevertheless the preferred treatment option in some clinical scenarios.[22]
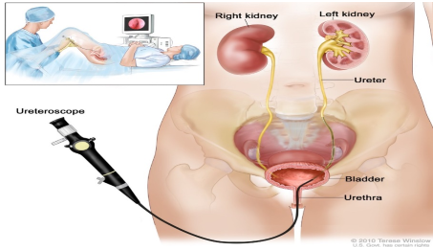
Ureterorenoscopy
Flexible ureteroscopes are required for endoscopic treatment of kidney stones through natural orifices. Numerous data from randomized controlled trials have demonstrated the excellent success rates of ureteroscopy in treating ureteric stones. Better results from this method include a reduced rate of re-interventions, fewer sick leave days, fewer stone-free rates following treatment, and cheaper healthcare costs. Nephrolithotomy Percutaneous (PCNL): Since its introduction by Fernström and Johansson in 1976, PCNL has proven to be a successful alternative to open surgery when treating renal stones larger than 2 mm or lower pole stones larger than 1 mm. However, patients undergoing ureteroscopy may still have leftover stone pieces, which puts them at risk for infection, recurring symptoms, and longer hospital admissions than those undergoing ESWL and PCNL.[23]
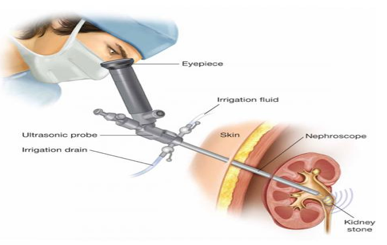
Percutaneous nephrolithotomy
It is the recommended treatment choice for staghorn calculi, with a stone-free rate of 85% to 93%. Contraindications to PCNL use include pregnancy, bleeding disorders, and uncontrolled UTIs.[24]
Electronic Endoscopes
At the beginning of this century, ureteroscopy received a new impulse thanks to novel technological refinements such as miniaturization of scope profile, improved maneuverability, and optimized accessory instrumentation. Currently available flexible ureteroscopes have an average tip diameter of about 6.9–7.5 Fr and a mid-shaft diameter of 7.5–9.0 Fr and can be inserted in an intramural ureter without active dilation in most cases. Image quality was also improved by incorporating an optical chip such as a CMOS (complementary metal oxide semiconductor) or CCD (charge-couple device) at the tip of the ureteroscope together with distal LED light and image processing capabilities. Digital ureteroscopes eliminate the honeycomb effect, and deflection is comparable to traditional fiber-optic endoscopes. In September 2006, Gyrus-ACMI (Southboro, Massachusetts, USA) was the first to introduce a ureteroscope incorporating this technology: the DUR-D ureteroscope.[25], [26]

Conclusion
In conclusion, this comprehensive review paper has provided an overview of novel concepts about the mechanisms underlying stone development. We gathered the latest research on metabolic risk factors, receptors, promoters, and inhibitors associated with kidney stone disease. It is evident that kidney stone disease has a more complex pathophysiology than only crystallization mechanisms. The need to evaluate the efficacy of imaging modalities for stone diagnosis has been underscored by changes in stone composition and the increased incidence of urolithiasis in recent decades. The study did not address these unresolved issues. Computed tomography (CT) scans have remained the gold standard imaging modality due to their superior sensitivity and specificity in identifying stones, as well as their time and cost-effectiveness. However, it's crucial to be aware of the radiation risk associated with CT scans, particularly for individuals who are prone to recurrent stone episodes, expectant mothers, and children. Combining kidney-ureter-bladder (KUB) x-rays and ultrasound (US) has been shown to be a good way to find ureteral stones while keeping costs and radiation exposure to a minimum. Additionally, in emergencies, bedside ultrasonography may be used to rapidly assess obstructive hydronephrosis in patients with suspected urolithiasis. The need for radiologists to use alternative imaging modalities grows as they attempt to minimize radiation exposure from CT and fluoroscopy.
Source of Funding
None.
Conflict of Interest
None.
References
- T Vijaya, M S Kumar, N V Ramarao, A N Babu, N Ramarao. Urolithiasis and Its Causes - Short Review. J Phytopharmacol 2013. [Google Scholar]
- T Alelign, B Petros. Kidney Stone Disease: An Update on Current Concepts. Adv Urol 2018. [Google Scholar]
- T Alelign. Kidney Stone Disease: An Update on Current Concepts. Adv Urol 2018. [Google Scholar]
- T Alelign. Kidney Stone Disease: An Update on Current Concepts. Adv Urol 2018. [Google Scholar]
- KK Malhotra. Medical aspects of renal stone. J Indian Acad Clin Med 2008. [Google Scholar]
- . Kidney Stone Disease: An Update on Current Concepts. Tilahun Alelign and Beyene Petros Review Article . [Google Scholar]
- Orson W. . Kidney Stone Pathophysiology and Medical Management 2006. [Google Scholar]
- S K Pareta. Establishing the Principle of Herbal Therapy for Antiurolithiatic Activity: A Review. J Pharmacol Toxicol 2011. [Google Scholar]
- A A Shokeir. Renal Colic: New Concepts Related to Pathophysiology, Diagnosis and Treatment. Curr Opin Urol 2002. [Google Scholar]
- . Recent advances on the mechanisms of kidney stone formation (Review). Int J Mol Med 2021. [Google Scholar]
- T Vijaya, M S Kumar, N V Ramarao, A N Babu, N Ramarao. Urolithiasis and Its Causes - Short Review. J Phytopharmacol 2013. [Google Scholar]
- . . Role of Dietary Supplements in Prevention of Renal Stones: An Update . [Google Scholar]
- D R Smith. . General Urology. Lange Medical Publications . [Google Scholar]
- Z Wang. Recent advances on the mechanisms of kidney stone formation (Review). Int J Mol Med 2021. [Google Scholar]
- Basavaraj, C S Biyani, A J Browning, J J Cartledge. The Role of Urinary Kidney Stone Inhibitors and Promoters in the Pathogenesis of Calcium Containing Renal Stones. Beau-Ebu Update Ser 2007. [Google Scholar]
- S Bawari, AN Sah, D Tewari. Urolithiasis: An Update on Diagnostic Modalities and Treatment Protocols. Indian J Pharm Sci 2017. [Google Scholar]
- A A Shokeir. Renal Colic: New Concepts Related to Pathophysiology, Diagnosis and Treatment. Curr Opin Urol 2002. [Google Scholar]
- Y Andrabi, M Patino, C J Das, B Eisner, D V Sahani, A Kambadakone. Advances in CT imaging for urolithiasis. Indian J Urol 2015. [Google Scholar]
- W R Masch, K C Cronin, D V Sahani, A Kambadakone. Imaging in urolithiasis. Radiol Clin North Am 2017. [Google Scholar]
- F Regan, B Kuszyk, M E Bohlman, S Jackman. Acute ureteric calculus obstruction: unenhanced spiral CT versus HASTE MR urography and abdominal radiograph. Br J Radiol 2005. [Google Scholar]
- E Mazzucchi, M Srougi. What's new in the diagnosis and management of urinary lithiasis?. Rev Assoc Med Bras 1992. [Google Scholar]
- N Petrides, S Ismail, F Anjum, S Sriprasad. How to maximize the efficacy of shockwave lithotripsy. Turk J Urol . [Google Scholar]
- J Van Besien, P Uvin, I Hermie, T Tailly, L Merckx. Ultrasonography is not inferior to fluoroscopy to guide extracorporeal shock waves during treatment of renal and upper ureteric calculi: a randomized prospective study. Biomed Res Int 2017. [Google Scholar]
- W R Masch, K C Cronin, D V Sahani, A Kambadakone. Imaging in urolithiasis. Radiol Clin North Am 2017. [Google Scholar]
- D Canes, M M Desai. New technology in the treatment of nephrolithiasis. Curr Opin Urol . [Google Scholar]
- . . Geavlete P: flexible ureteroscopy: reshaping the upper urinary tract endourology 2011. [Google Scholar]
- Introduction
- Epidemiology of Kidney Stones
- Causes of Urinary Tract Stone Formation
- Symptoms and indicators of urolithiasis illnesses
- Kidney stone symptoms include
- Conventional treatment and prevention of urolithiasis diseases
- Surgical treatment likes
- Foods that enhance the risk of calculi formation
- Foods that inhibit calculi formation
- Available treatments
- Pathogenesis of renal stone formation
- Types of kidney stones
- Mechanisms of Renal Stone Formation
- Promoters of stone formation
- Inhibitors of stone formation
- Nucleation
- Crystal growth
- Aggregation
- Retention
- Pharmacological agents used for the treatment of urolithiasis
- Diagnostic Techniques
- Ultrasonography
- Magnetic Resonance Urography
- Management
- Extracorporeal Shock Wave Lithotripsy (ESWL)
- Ureterorenoscopy
- Electronic Endoscopes
- Conclusion
- Source of Funding
- Conflict of Interest
