- Visibility 0.9k Views
- Downloads 44 Downloads
- Permissions
- DOI 10.18231/j.ijcaap.2020.036
-
CrossMark
- Citation
A systematic review on wound healing and its promising medicinal plants
- Author Details:
-
Sofia Khanam *
Abstract
Wound healing is one of the most complex and dynamic processes in the body of the human. Wound healing is an essential biological development to sustain the integrity of skin after trauma, either by accident or by a deliberate process. In the phases of hemostasis, inflammation, development, re-epithelialization, and remodeling, this includes the spatial and temporal coordination of many cell types with different functions. In understanding the mechanisms of normal wound closure, it is important to unravel the functions of these cell types and their interactions with each other. Micro-environmental changes, including changes in mechanical forces, levels of oxygen, chemokines, extracellular matrix, and synthesis of growth factor, directly influence cellular recruitment and activation, leading to disrupted wound healing conditions. Wounds are cured with different medicinal plants or from their extracts. Plants supply humans with different medicines, and medicinal plants are the blessing of nature used to heal wounds with even lower side effects. This systematic review aims to explain the physiology of the wound healing process, different cellular, and molecular aspects, and to provide insight into the various plants that have possible wound healing properties that could be valuable in healing practice.
Introduction
In the human body, the skin is the largest organ by surface area. It is the essential structure that shields mechanical injury, ultraviolet radiation, microbial infection, and intense temperature from internal tissues. Wounds are serious cases of physical disability.[1] A wound that is caused by human, biological, immunological, microbial injury, or usually associated with lost function disrupted tissue condition. It can lead to pain, discomfort, inflammation, infection, and occasionally organ failure if the wound stays untreated. [2] Wound healing is a complex and complicated mechanism involving a sequence of arranged events, including bleeding, clotting, initiation of an acute inflammatory response to initial damage, regeneration, migration, and proliferation of connective tissue and parenchyma cells, as well as extracellular matrix protein synthesis, remodeling of new parenchyma and connective tissue, and deposition of collagen. Finally, it takes place in an orderly fashion to improve the wound strength and culminates in the reconstruction of severed tissues. [3], [4] It involves continuous cell-cell and cell-matrix interactions that allow the mechanism to continue in diverse overlapping phases and processes including inflammation, wound contraction, Re epithelialization tissue, remodeling, & angiogenesis granulation tissue formation. [5] In particular, diabetic patients, the elderly, and patients with inherited diseases such as sickle cell disease are predisposed to irregular healing of wounds resulting in long-term sequelae. The measures that exist, unexpectedly, have not dramatically impacted the situation. Although there are many treatments available for wound healing, these are only marginally effective. There is thus a need for more efficient wound healing therapies. [6] In the process of wound healing, many medicinal plants have a very significant role. Plants are more effective healers because they inherently facilitate recovery mechanisms. [7] Plant-based treatment not only speeds up the process of regeneration but also preserves aesthetics. More than 70% of preparation wound treatment drugs are plant-based, 20% are mineral-based and the rest contain animal products as their base content. The plant-based materials are used as first aid – antiseptic coagulants and wound wash. Therapeutic plants show wound healing properties by the different mechanisms, such as wound healing modulation, declining bacterial count, refining collagen deposition, increasing fibrocytes and fibroblasts, etc. In recent ages, the focus on plant researchers has increased all over the world and a wide-ranging body of evidence has been collected to show the immense potential of medicinal plants used in various traditional systems. More than 13,000 plants have been studied during the last five years period. [8], [9], [10]
|
Classification of Wounds |
|
|
1. Based on the intensity of the wound |
|
|
Simple Wound |
Complex Wound |
|
In this type, the injury and impairment are only to the skin.[11] |
In this type, the wound comprises fundamental tissues, tendons, muscles, etc. [11] |
|
2. Based on the nature of the wound |
|
|
Open Wound |
Closed Wound |
|
An open wound is a disruption or breakdown on the surface of the skin that can cause bleeding externally and allow bacteria to invade the body, causing an infection such as abrasions, contusions, incision, hematoma, laceration, etc. [12] |
A closed wound occurs after a blunt force impacts the body, such as lacerated, incised, crushed & piercing. [13] |
|
3. Based on the physiology of wound |
|
|
Acute Wound |
Chronic Wound |
|
Those wounds that are healed in a brief period and go through a sequence of steps needed for wound healing to restore the anatomical integrity of the wounded site, such as wound due to cut & surgical injury. [14] |
These types of wounds take a long time for their healing. For example trauma, loss of oxygen supply, local infection, diseases such as nutritional deficiency, diabetes, and medication may contribute to the growth of chronic wounds. [15] |
|
S No. |
Phases |
Time of phase |
Cells involved |
Functions |
|
|
1 |
Hemostasis |
Immediate |
Platelets |
Stop bleeding |
|
|
2 |
Inflammation |
2-5 days Some cases (2 weeks) |
Neutrophils Macrophages |
Elimination of cell debris and infection-causing agents |
|
|
3 |
Proliferation |
3 days to 2 weeks |
Lymphocytes Fibroblasts Keratinocytes |
Formation of granulation tissue, angiogenesis |
|
|
4 |
Remodelling |
21 days to 2 years |
Fibroblasts |
Collagen formation & scar maturation |
Types of wounds
Wounds are categorized into 3 classes i.e. intensity of the wound, based on the nature of the wound, and physiology of the wound ([Table 1]).
Wound Healing Process
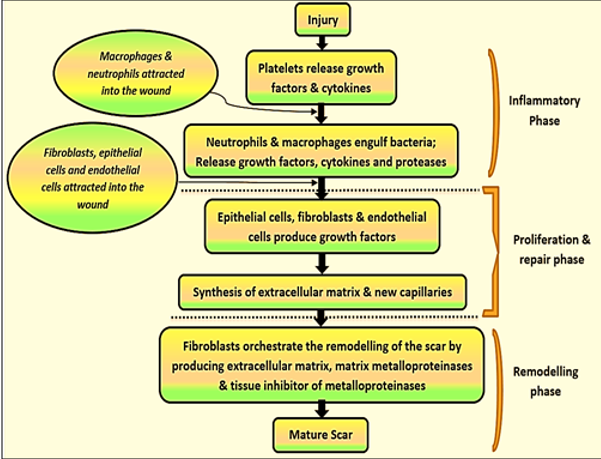
Wounding and wound healing occurs in all the body's tissues and organs. Many of these mechanisms of restoration are prevalent in all tissues. While the healing process is ongoing, to better explain the physiological processes taking place in the wound and underlying tissue, it is randomly separated into distinct stages. [24] Healing is a dynamic mechanism involving interactions between different immunological and biological processes that are co-ordinated. During different stages of the healing process, it requires a cascade of closely and specifically controlled steps and activities that coincide with the appearance of different cell types in the wound bed. The multiple processes in acute tissue recovery, which are caused by tissue damage, can be united into a sequence of four time-dependent phases viz. Hemostasis, Inflammation, Proliferation & Remodelling ([Figure 1] &[Table 2]).[25], [26]
Hemostasis
If the skin is injured, vasoconstriction of the vessel walls is the automatic reaction to stop bleeding. Next, two concurrent and mechanistically interconnected pathways contribute to primary hemostasis and secondary hemostasis. [27] Primary hemostasis requires platelet accumulation and the development of platelet plugs caused by collagen exposure within the sub-endothelial matrix. Secondary hemostasis refers to the coagulation cascade activation where soluble fibrinogen is turned into insoluble strands that make up the mesh of fibrin. The platelet plug and the fibrin mesh combine to form a thrombus that stops bleeding, releases accompaniments and growth factors, and provides a temporary scaffold for infiltrating cells that are necessary for wound healing. [28]
Inflammation
The inflammatory process occurs shortly after the injury, which typically lasts between 24 and 48 hours and may, in some cases last for up to 2 weeks. The inflammatory phase initiates hemostatic pathways immediately to stop the bleeding from the site of the wound. As a result, clinically identifiable cardinal signs of inflammation, redness of the skin, color, tumor, pain, and functio-laesa emerge. Vasoconstriction and platelet aggregation to cause blood clotting and consequently, vasodilatation and phagocytosis to produce inflammation at the wound site are distinguished by this process.[29]
Proliferation
The acute wound moves toward tissue healing after persistent damage has ceased, hemostasis has been reached and an immune system has been successfully set in place. [30], [31] The proliferative process begins the following damage on the third day and continues for about 2 weeks afterward. It is characterized by fibroblast migration and newly synthesized extracellular matrix deposition, serving as a substitute for the fibrin and fibronectin provisional network. This process of wound healing can be seen at the macroscopic stage as an abundant development of granulation tissue. [32]
Remodeling
The granulation tissue undergoes a slow declining period in this last step of wound healing. The skeletal muscle epidermis, dermal vasculature, nerves, and myofibers are remodeled, developing functional tissue.[33] Vascular elements of the granulation tissue fibroblast and myofibroblast are diminished and PBMC cells undergo apoptosis or exit the wound. Similarly, there is a decline in the amounts of glycosaminoglycans and proteoglycans that play a structural and hydration role.[34] Collagen metalloproteinases produced by fibroblasts and macrophages dissolve and replace Type III collagen of the granulation tissue with Type I collagen, which is further reorganized into parallel fibrils, producing a scar of low cellularity. This last stage will last for months.[35], [36]
Physiology of Wound Healing
The wound healing phase consists mostly of four steps viz. hemostasis, inflammation, proliferation, and remodeling. After the wound, hemostasis instantly begins which is accompanied by inflammation. It includes constriction of the blood vessels, migration of platelets to the wounded site, blood coagulation by the release of multiple factors such as platelet-derived growth factor (PDGF) and transforming other growth factor-beta (TGF-β) and other factors of chemo-attractant produced by injured parenchymal cells. The inflammation is then accompanied by a proliferative process. [37] It facilitates the proliferation of cells such as fibrocytes, platelets, mesenchymal cells, and endothelial cells required for tissue regeneration and angiogenesis capillary regrowth (formation of new blood vessels by endothelial cell construction) to increase the blood supply to the injured cells. Angiogenesis, fibroplasia & epithelisation are the repair processes at this period. The final step of wound healing is the Maturation & remodeling process leading to maturation & scar-forming by generating MMP's (Matrix metalloproteinases), ECM (Extracellular matrix), and TIMP's (Tissue inhibitor of metalloproteinases). Myofibroblasts facilitate wound contracting and the synthesis of all these steps results in wound healing with the development of matured scar ([Figure 2]).[38]
Factors influencing wound healing
The two types of factors influencing wound healing- Local & Systematic factors. [39]
Local factors
Local factors include infection by the organization of tissue that interrupts healing, exposure to ultraviolet light facilities curing, movement of the affected part of the healing delay, poor blood supply which shows delay in healing, exposure to ionizing radiation delay granulation, foreign bodies including sutures interferes in healing. [40]
Systematic factors
Systematic factors comprise diabetics are more prone to infection and hence delay healing, wound healing is speedy in young and slow in aged people, hematological aberrations also disturbs healing, administration of glucocorticoids (anti-inflammatory) interrupt healing, nutritional deficiency of vitamin C and zinc delay healing. [41]
Wound healing management by medicinal plants
For the management of wound healing, various treatments are used. To assist wound recovery, multiple therapies were used locally and systematically. Several agents are used for wound healing, including antibiotics and antiseptics, desloughing agents’ viz. hydrogen peroxide, wound healing promoters, eusol and collagenase ointment, some compounds such as extracts, minerals, vitamins, and a variety of plant products. Medicinal plants heal the healing process of wounds by facilitating blood clotting, combating inflammation, and speeding up wound healing. Plants and chemical agents collected from plants can be recorded to facilitate care and maintain wound healing. Medicinal plants demonstrate wound healing effects by various pathways, such as wound healing modulation, reduced bacterial count, enhanced deposition of collagen, increased fibroblasts and fibrocytes, etc. [42]
It has been documented that several medicinal plants demonstrate wound healing activity. Extensive research has been carried out in the area of medicinal plant wound healing treatment. The following are several recent research on medicinal plants with important wound healing activity are recapitulated in the tabular form (Table 3).
|
S. No |
Medicinal plants |
Family |
Part used |
Bioactive Constituents |
Uses |
Ref |
|
1 |
Aloe Barbadensis (Aloe vera) |
Aloaceae |
Leaves, latex |
Aloe-emodin, barbaloin. |
Wound Healing |
|
|
2 |
Artemisia pallens (Davana, Davanum) |
Asteraceae |
Whole plant |
Davanone, davan ether, davana, furanand linalool. |
Cuts & wounds |
|
|
3 |
Lawsonia alba (Heena) |
Lythraceae |
Leaf |
Lawsonecoumarins, xanthones, flavonoids, naphthoquinines, steroids, fatty acid. |
Wounds |
|
|
4 |
Pterocarpus santalinus (Lal Chandan) |
Fabaceae |
Leaf, stem |
Phenols, anthocyanin, saponin, triterpenoids, flavonoids, tannins, glycerides, glycosides, |
Cuts, wounds, boils, inflammation |
|
|
5 |
Morinda citrifolia (Indian mulberry) |
Rubiaceae |
Leaves |
Scopoletin, catechin, beta-sitosterol, damnacanthal, alkaloids, lignans |
Wounds |
|
|
6 |
Sesamum indicum (Til) |
Pedaliaceae |
Roots |
Sesame seeds (up to 60% oil), 30% protein, vitamin E, B-complex vitamins (niacin), folic acid, magnesium, phosphorous, calcium, |
Wounds |
|
|
7 |
Acalypha langiana (Khokali) |
Euphorbiaceae |
Leaves |
Acalyphine and triacetoneamine, cyanogenic glucosides, and alkaloids. |
On external wounds |
|
|
8 |
Vernonia arborea (Karana, Sadagai) |
Asteraceae |
Leaves, bark |
Alpha-amyrin acetate, beta-amyrin, lupeol, stigmasterol, beta-sitosterol |
Wounds |
|
|
9 |
Cassia fistula (bendra, lathi) |
Fabaceae |
Leaves |
Anthraquinones, fistulic acid, rhein, rheinglucoside, sennosoides A and B, phlobaphenes, lupeol, emodin, chrysophanic acid, beta-sitosterol and hexacosanol, fistuacacidin, |
Wounds |
|
|
10 |
Abrus precatorius (Gunchi, gunja) |
Fabaceae |
Leaves |
Glycyrrhizin, Triterpene glycosides, pinitol, and alkaloids such as asabrine, hepaphotine, choline and precatorine |
Cuts & wounds |
|
|
11 |
Tragia involucrate (bichchuti) |
Euphorbiaceae |
Roots |
Tannins, flavanoids, alkaloids, saponins |
Pain, wounds, swellings, Eczema |
|
|
12 |
Alternanthera sessilis (chanchi) |
Amaranthaceae |
Leaves |
Stigmasterol, campesterol, B-sitosterol, a-stigmasteanol and also contain 5-a-stigmasta-7-enol. |
Antibacterial, wound healing |
|
|
13 |
Allium cepa (onion) |
Liliaceae |
Bulb |
Kampferol, β -sitosterol, ferulic acid, myritic acid, prostaglandins. |
Enhanced wound healing and Antibacterial property |
|
|
14 |
Curcuma longa (Turmeric, Haldi) |
Zingiberaceae |
Rhizomes |
Curcumin (diferuloylmethane), turmeric oil or turmerol & 1, 7-bis, 6- hepta-diene-3, 5-Dione. |
would healing and regeneration |
|
|
15 |
Mimusops Elengi (Bakul) |
Sapotaceae |
Barks |
taraxerol, taraxerone, ursolic acid,betulinic acid, V-spinosterol, W-sitosterol, lupeol, alkaloid isoretronecyl tiglate & mixture of triterpenoid saponins |
Stimulated wound contraction; increase the tensile strength of incision |
Conclusion
Wound healing is a process that begins with trauma and concludes with the formation of scars. Wound treatment aims to increase the healing process and decrease the risk factors. Plants are more potent healers because they facilitate the repair mechanism naturally. This research revealed that traditional medicines are still used by tribal people and the importance of a large number of plants used in tribal medicine, especially for wound healing, is determined. Knowledge of plants for the treatment of different diseases, including wounds, is still seemingly uncertain. These natural plants are a rich focus on the production of synthetic drug alternatives. With fewer side effects, the synthesis of conventional and new expertise will create stronger medicines for wound healing. However, clinical confirmation, standardization, and safety evaluations of conventional medicinal plants are required before they can be approved for wound healing.
Conflicts of Interest
The author had no conflicts of interest to declare relative to this review.
References
- Nagori B, Solanki R. Role of Medicinal Plants in Wound Healing. Res J Med Plant. 2011;5(4):392-440. [Google Scholar] [Crossref]
- Kumar B, Vinaykumar M, Govindarajan R, Pushpangadan P. Ethanopharmacological approaches to wound healing exploring medicinal plants of India. J Ethanopharmacology. 2007;114:103-13. [Google Scholar]
- Rivera A, Spencer J. Clinical aspects of full-thickness wound healing. Clin Dermatol. 2007;25(1):39-48. [Google Scholar] [Crossref]
- Strecker-McGraw M, Jones T, Baer D. Soft Tissue Wounds and Principles of Healing. Emerg Med Clin North Am. 2007;25(1):1-22. [Google Scholar] [Crossref]
- Martin P. Wound healing - Aiming for perfect skin regeneration. Sci. 1991;276(5309):75-81. [Google Scholar]
- Fife CE, Carter MJ. Wound Care Outcomes and Associated Cost Among Patients Treated in US Outpatient Wound Centers: Data From the US Wound Registry. Wounds. 2012;24:10-7. [Google Scholar]
- Shenoy C, Patil MB, R. Preliminary phytochemical investigation and wound healing activity of Allium Cepalin (Liliaceae). Int J Pharm Pharm Sci. 2009;2(2). [Google Scholar]
- Biswas TK, Mukarjee B. Plant medicine as Indian origin for wound healing activity: A Review. Int J Lower Extremity Wounds. 2003;2:25-36. [Google Scholar]
- Dahanukar SA, Kulkarni RA, Rege NN. Pharmacology of medicinal plants and natural products. Indian J Pharm. 2000;32:81-118. [Google Scholar]
- Kumar B, Govindarajan M, Pusphagandan R. Ethanopharmacological approaches to wound healing-Exploring medicinal plants of India. J Ethanopharmacology. 2007;114(2):103-13. [Google Scholar]
- Bhargavi S, Kumar A, Babu R. Ancient and Modern View of Wound Healing: Therapeutic Treatments. Res J Pharm, Biol Chem Sci. 2011;2(3):474-93. [Google Scholar]
- Kumar A, Kumar P, Babu R. Review Article of Ancient and Modern View of Wound Healing: Therapeutic Treatments. Res J Pharm, Biol Chem. 2011;2. [Google Scholar]
- Lazarus G, Cooper D, Knighton D, Margolis D, Percoraro R, Rodeheaver G. Definitions and guidelines for assessment of wounds and evaluation of healing. Arch Dermatol. 1994;130:489-93. [Google Scholar] [Crossref]
- Menke N, Ward K, Witten T, Bonchev D, Diegelmann R. Impaired wound healing. Clin Dermatol. 2007;25(1):19-25. [Google Scholar] [Crossref]
- Alam G, Singh MP. Wound healing potential of some medicinal plants. Int J Pharm Sci Rev Res. 2011;9:136-45. [Google Scholar]
- Guo S, Dipietro LA. Critical review in oral biology & medicine: factors affecting wound healing. J Dent Res. 2010;89(3):219-29. [Google Scholar]
- Robson MC. Cytokine manipulation of the wound. Clin Plastic Surg. 2003;30(1):57-65. [Google Scholar] [Crossref]
- Wu Y, Chen S. Apoptotic cell: linkage of inflammation and wound healing. Front Pharmacol. 2014;5(1). [Google Scholar]
- Koh T, DiPietro L. Inflammation and wound healing: the role of the macrophage. Exp Rev Mol Med. 2011;13(e23):1-12. [Google Scholar] [Crossref]
- Dulmovits B, Herman I. Microvascular remodeling and wound healing: A role for pericytes. Int J Biochem Cell Biol. 2012;44(11):1800-12. [Google Scholar] [Crossref]
- Li B, Wang JC. Fibroblasts and myofibroblasts in wound healing: force generation and measurement. J Tissue Viability. 2011;20(4):108-20. [Google Scholar]
- Gurtner G, Werner S, Barrandon Y, Longaker M. Wound repair and regeneration. Nat. 2008;453(7193):314-21. [Google Scholar] [Crossref]
- Reinke J, Sorg H. Wound Repair and Regeneration. Euro Surg Res. 2012;49(1):35-43. [Google Scholar] [Crossref]
- Richardson M. Acute wounds: an overview of the physiological healing process. Nurs Times. 2004;100:50-3. [Google Scholar]
- Vanwijck R. Surgical biology of wound healing. Belgique (Brussels). 2001;115:175-84. [Google Scholar]
- Degreef H. How to heal a wound fast. Dermatol Clin. 1998;16(2):365-75. [Google Scholar] [Crossref]
- Furie B, Furie B. Mechanisms of Thrombus Formation. N Engl J Med. 2008;359(9):938-49. [Google Scholar] [Crossref]
- Pool JG. Normal hemostatic mechanisms: a review. Am J Med. 1977;43:776-80. [Google Scholar]
- Li J, Chen J, Kirsener R. Pathophysiology of acute wound healing. Clin Dermatol. 2007;25:9-18. [Google Scholar]
- Hart J. Inflammation 1: its role in the healing of acute wounds. J Wound Care. 2002;11(6):205-9. [Google Scholar] [Crossref]
- Skover GR. Cellular and biochemical dynamics of wound repair. Wound environment in collagen regeneration. Clin Podiatric Med Surg. 1991;8:723-56. [Google Scholar]
- Flangan M. The physiology of wound healing. J Wound Care. 2000;9:299-300. [Google Scholar]
- Olczyk P, Mencner �, Komosinska-Vassev K. The Role of the Extracellular Matrix Components in Cutaneous Wound Healing. Bio Med Res Int. 2014. [Google Scholar] [Crossref]
- Wynn T, Vannella K. Macrophages in Tissue Repair, Regeneration, and Fibrosis. Immun. 2016;44(3):450-62. [Google Scholar] [Crossref]
- Novak ML, Koh T. Phenotypic Transitions of Macrophages Orchestrate Tissue Repair. Am J Pathol. 2013;183(5):1352-63. [Google Scholar] [Crossref]
- Maquart F, Monboisse J. Extracellular matrix and wound healing. Pathol Biol. 2014;62(2):91-5. [Google Scholar] [Crossref]
- Sabale P, Bhimani B, Prajapati. An overview of medicinal plants as wound healers. J Appl Pharm Sci. 2012;2:143-50. [Google Scholar]
- Barrientos S, Stojadinovic O, Golinko M, Brem H, Tomic-Canic M. PERSPECTIVE ARTICLE: Growth factors and cytokines in wound healing. Wound Rep Regen. 2008;16(5):585-601. [Google Scholar] [Crossref]
- Hess T. Checklist for factors Affecting Wound Healing. Adv Skin Wound Care. 2011;24. [Google Scholar]
- AMR, Vieira BJ, Andrade LCFd, Aarestrup FM. Effects of low-level laser therapy on the progress of wound healing in humans: the contribution of in vitro and in vivo experimental studies. J Vasc Bras. 2007;6(3):258-66. [Google Scholar] [Crossref]
- Sibbald RG, Woo K, Ayello EA. Increased Bacterial Burden and Infection. Adv Skin Wound Care. 2006;19(8):447-61. [Google Scholar] [Crossref]
- Raina R, Prawez S, Verma PK, Pankaj NK. Medicinal plants and their role in wound healing. Vet Scan. 2008;3(1):1-24. [Google Scholar]
- Patil H, Dattatraya K. Review Article Pterocarpus Marsupium: A valuable medicinal plant in diabetes management. Int J Appl Biol Pharm Technol. 2011;2:976-4550. [Google Scholar]
- Rajagopal PL, Premaletha K, Kiron SS, Sreejith KR. Phytochemical and Pharmacological Review on Cassia fistula Linn. – “The Golden Shower”.. Int J Pharm, Chem Biol Sci. 2013;3(3):672-9. [Google Scholar]
- Haque A, Hassan M, Das A, Begum B, Ali Y. Phytochemical investigation of Vernonia cinerea (Family: Asteraceae). J Appl Pharm Sci. 2012;2(6):79-83. [Google Scholar]
- Ayyanar M, Ignacimuthu S. Herbal medicines for wound healing among tribal people in Southern India: Ethnobotanical and Scientific evidences. Int J Appl Res Nat Prod. 2009;2(3):29-42. [Google Scholar]
- Brazzaville C, Nzikou M, Matos G, Kalou B. Chemical Composition on the Seeds and Oil of Sesame (Sesamum indicum L.). Adv J Food Sci Technol. 2009;1(1):6-11. [Google Scholar]
- Galal EE, Gawad MA. Antidiabetic activity of Egyptian onion Allium cepa extract. J Egypt Med Assoc. 1965;48:14-45. [Google Scholar]
- Nizamuddin, Bin S. International centre for chemical and biological sciences. . 2013;35. [Google Scholar]
- Pujar P, Sawaikar D, Rojatkar S, Nagasampagi B. A new germacranolide from Artemisia pallens. J Pharm. 2000;71(5):590-2. [Google Scholar] [Crossref]
- Ilango K, Chitra V. Wound healing and anti-oxidant activities of the fruit pulp of limonia acidissima linn (rutaceae) in rats. Trop J Pharm Res. 2010;9(3):223-30. [Google Scholar] [Crossref]
- Sajithlal GB. Influence of aloe vera on collagen turnover in healing of dermal wounds in rats. Indian J Exp Biol. 2000;36:896-901. [Google Scholar]
- Subhashini T, Krishnaveni B, Reddy S. Anti-inflammatory activity of leaf extract of Alternanthera sessilis. Hygeia J Drugs Med. 2010;2(1):54-6. [Google Scholar]
- Srimal RC, Khanna NM, Dhawan BN. A preliminary report on anti-inflammatory activity of Cucurmin. Indian J Pharmacol. 1971;3. [Google Scholar]
- Misra G, Mitra C. Constituents of fruit and seed of Mimusops elengi. Phytochemistry. 1967;6(3). [Google Scholar] [Crossref]
- Rao V. Pharmacological evaluation of root extracts of tragia involucrata. Int J Pharm Sci Drug Res. 2007. [Google Scholar]
- Anam E. Anti-inflammatory activity of compounds isolated from the aerial parts of Abrus precatorius (Fabaceae). Phytomed. 2001;8(1):24-7. [Google Scholar] [Crossref]
- Morton J. The ocean-going noni, or Indian Mulberry (Morinda citrifolia, Rubiaceae) and some of its “colorful” relatives. Economic Botany. 1992;149(4):1899-908. [Google Scholar]
How to Cite This Article
Vancouver
Khanam S. A systematic review on wound healing and its promising medicinal plants [Internet]. IP Int J Compr Adv Pharmacol. 2020 [cited 2025 Nov 09];5(4):170-176. Available from: https://doi.org/10.18231/j.ijcaap.2020.036
APA
Khanam, S. (2020). A systematic review on wound healing and its promising medicinal plants. IP Int J Compr Adv Pharmacol, 5(4), 170-176. https://doi.org/10.18231/j.ijcaap.2020.036
MLA
Khanam, Sofia. "A systematic review on wound healing and its promising medicinal plants." IP Int J Compr Adv Pharmacol, vol. 5, no. 4, 2020, pp. 170-176. https://doi.org/10.18231/j.ijcaap.2020.036
Chicago
Khanam, S.. "A systematic review on wound healing and its promising medicinal plants." IP Int J Compr Adv Pharmacol 5, no. 4 (2020): 170-176. https://doi.org/10.18231/j.ijcaap.2020.036
